Des bouffées de chaleur qui perturbent vos réunions de travail ? Des sueurs nocturnes qui vous empêchent de dormir ? Vous n’êtes pas seule : 80 % des femmes souffrent de ces symptômes gênants pendant la ménopause, et les traitements hormonaux de substitution (THS) deviennent la solution privilégiée pour les soulager [13]. Les chiffres sont éloquents : le NHS a prescrit 13 millions de traitements THS à 2,6 millions de patientes en Angleterre en 2023/24, contre un peu moins de 11 millions de traitements pour 2,3 millions de femmes l’année précédente [13].
L’hormonothérapie substitutive (HTS) s’attaque directement aux symptômes gênants comme les bouffées de chaleur et les sueurs nocturnes, apportant souvent un soulagement en quelques semaines [13]. Mais ses bienfaits ne se limitent pas au contrôle des symptômes : les options d’HTS disponibles au Royaume-Uni contribuent à prévenir la perte osseuse et à réduire le risque de fracture [13] [12]. Bien que des inquiétudes subsistent quant au risque de cancer du sein [13], de nombreuses études montrent que, pour la plupart des femmes, les bénéfices de l’HTS surpassent largement les risques potentiels [12].
Ce guide vous explique tout ce que vous devez savoir sur les avantages, les effets secondaires et les options de traitement hormonal substitutif (THS) au Royaume-Uni. Que vous commenciez tout juste à ressentir les premiers symptômes de la périménopause ou que vous soyez déjà à la recherche d'un traitement, vous trouverez des informations fondées sur des preuves scientifiques pour vous aider à prendre la meilleure décision concernant le THS durant cette importante période de transition.
Qu’est-ce que le traitement hormonal de la ménopause et comment fonctionne-t-il ?
Le traitement hormonal substitutif (THS) agit en remplaçant les hormones que votre corps produit en moindre quantité à l'approche et pendant la ménopause . Ce traitement médical s'attaque à la cause profonde des symptômes de la ménopause en rétablissant les taux d'hormones qui ont naturellement diminué au cours de cette importante transition de vie.
Comprendre les changements hormonaux pendant la ménopause
Avec l'âge, la production d'hormones par les ovaires diminue. Ce phénomène survient généralement chez les femmes âgées de 45 à 55 ans [13], bien que certaines connaissent une ménopause précoce ou induite plus tôt suite à des interventions médicales comme l'hystérectomie.
Durant la périménopause , les ovaires deviennent moins sensibles aux signaux de contrôle de l'hypophyse, notamment à l'hormone folliculo-stimulante (FSH) et à l'hormone lutéinisante (LH) [9]. Il en résulte une baisse de la production d'œstrogènes et de progestérone, à l'origine des fluctuations hormonales responsables des symptômes physiques et émotionnels gênants.
La chute du taux d'œstrogènes entraîne de multiples changements dans tout votre corps :
-
Augmentation du stockage des graisses abdominales centrales
-
Résistance à l'insuline, augmentation du risque de diabète de type 2
-
Altération de la fonction vasculaire et profils de cholestérol défavorables
-
Perte osseuse accélérée, commençant même avant vos dernières règles [9]
Des études montrent que 40 à 60 % des femmes consultent pour des symptômes de la ménopause, tandis que 20 % retardent leur traitement pendant plus d'un an [9]. Même les femmes plus âgées ne sont pas épargnées : 42 % des femmes âgées de 60 à 64 ans et 33 % de celles âgées de 65 à 79 ans souffrent encore de bouffées de chaleur et de sueurs nocturnes [9].
Quelles hormones sont remplacées dans le cadre d'un traitement hormonal de substitution (THS) ?
Le THS se concentre sur deux hormones clés : les œstrogènes et la progestérone. Outre la reproduction, ces hormones soutiennent des fonctions essentielles comme la solidité osseuse et la santé cardiaque [13].
Vos options de traitement comprennent :
Traitement hormonal substitutif (THS) à base d'œstrogènes seuls : conçu spécifiquement pour les femmes ayant subi une hystérectomie [13]. En l'absence d'utérus à protéger, les œstrogènes seuls permettent de gérer efficacement les symptômes.
Traitement hormonal substitutif combiné : essentiel pour les femmes ayant un utérus intact, il associe œstrogènes et progestatifs [13]. Le progestatif prévient la prolifération anormale de la muqueuse utérine que les œstrogènes seuls pourraient provoquer [10].
Différentes formes d'œstrogènes sont disponibles :
-
Œstrogènes équins conjugués (mélange d'œstrogènes d'origine naturelle)
-
Œstrogènes conjugués de synthèse (y compris le sulfate d'œstrone)
-
17β-œstradiol micronisé (identique à l'œstradiol naturel de vos ovaires) [9]
La testostérone peut également être prescrite, bien qu'elle ne soit pas actuellement autorisée spécifiquement pour les symptômes de la ménopause au Royaume-Uni. Un spécialiste peut la prescrire lorsque cela est cliniquement justifié [13].
Comment le THS soulage les symptômes de la ménopause
Le THS (traitement hormonal substitutif) offre des résultats impressionnants en rétablissant des taux d'hormones proches de ceux produits antérieurement par votre corps. La plupart des femmes constatent un soulagement significatif de leurs symptômes dès le début du traitement [10]. Le THS agit efficacement sur :
-
Bouffées de chaleur et sueurs nocturnes , s’améliorant souvent en quelques semaines après le début du traitement [18]
-
Sécheresse vaginale et rapports sexuels douloureux
-
Sautes d'humeur , dépression et irritabilité
-
Troubles du sommeil et insomnie
-
brouillard cérébral et symptômes cognitifs
-
Problèmes urinaires, notamment les fuites.
Les avantages vont au-delà du contrôle des symptômes. Le THS protège la santé osseuse en prévenant l'ostéoporose et les fractures, ce qui est crucial puisque la baisse des œstrogènes peut entraîner une perte de densité osseuse allant jusqu'à un cinquième chez les femmes dans les cinq à sept ans suivant la ménopause [9].
Le THS peut également protéger contre les problèmes cardiovasculaires [9]. Des études indiquent que le rapport bénéfice-risque le plus favorable est obtenu lorsque le THS est débuté avant l’âge de 60 ans ou dans les 10 ans suivant la ménopause [13].
La plupart des femmes suivent un traitement hormonal substitutif (THS) pendant 2 à 5 ans, la durée variant selon les besoins individuels [13]. Les professionnels de santé surveillent et ajustent régulièrement les dosages afin d'optimiser les bénéfices tout en minimisant les risques potentiels.
Options de THS disponibles au Royaume-Uni
Il existe plusieurs options de THS pour soulager les symptômes de la ménopause , allant des comprimés pratiques aux patchs et gels cutanés. Aucune solution n'est universellement efficace ; bien comprendre les différentes options vous permettra de choisir le traitement le plus adapté, en concertation avec votre médecin.
Comprimés et THS oral
L’hormonothérapie substitutive orale offre une solution simple et économique, souvent privilégiée par les femmes. Ces comprimés à prendre quotidiennement contiennent soit des œstrogènes seuls, soit une association d’hormones, mais présentent un risque légèrement plus élevé de formation de caillots sanguins et d’AVC que les traitements transdermiques [12].
Deux principaux types de tablettes sont disponibles :
Les comprimés combinés à prise continue sont particulièrement adaptés aux femmes qui n'ont pas eu leurs règles depuis au moins 12 mois. Chaque comprimé contient à la fois un œstrogène et un progestatif et se prend quotidiennement sans interruption. Parmi les marques les plus courantes au Royaume-Uni, on trouve Kliofem, Kliovance et Femoston Conti [11].
Les comprimés combinés séquentiels conviennent aux femmes qui ont encore leurs règles ou dont les dernières règles remontent à moins de 12 mois. La prise quotidienne d'œstrogènes est associée à celle d'un progestatif pendant 10 à 14 jours à chaque cycle. Parmi les options courantes, on trouve Elleste Duet, Femoston et Novofem [11].
Patchs et applications cutanées
Les patchs libèrent les hormones progressivement à travers la peau, évitant ainsi tout contact avec le système digestif. Cela signifie qu'il n'y a pas de risque accru de formation de caillots sanguins, ce qui les rend plus sûrs que les comprimés pour de nombreuses femmes [4].
Les médecins recommandent particulièrement les patchs aux femmes présentant un risque élevé de thromboembolie veineuse (TEV) , notamment celles dont l'IMC est supérieur à 30 kg/m² [4]. Au Royaume-Uni, les options disponibles incluent Evorel, Estradot, Estraderm, FemSeven et Progynova [12].
Appliquez les patchs sur une peau propre et sèche sous la taille, en évitant la zone des seins [4]. La plupart des femmes les trouvent pratiques, bien que certaines puissent ressentir une légère irritation cutanée ou un décollement occasionnel pendant l'exercice [13].
Gels et sprays
Les gels et les sprays sont de plus en plus utilisés dans le cadre des traitements hormonaux substitutifs . Appliqués une fois par jour sur la peau, ils permettent aux hormones d'être progressivement absorbées par la circulation sanguine.
Vos principales options sont les suivantes :
-
Gels (Oestrogel, Sandrena) appliqués sur le haut des bras ou des cuisses [12]
-
Sprays (Lenzetto) vaporisés sur l'intérieur du bras ou de la cuisse [13]
Comme les patchs, ces traitements cutanés n’augmentent pas le risque de formation de caillots sanguins [13]. Laisser sécher les gels pendant 5 minutes et les sprays pendant 2 minutes avant de s’habiller [13]. Éviter tout contact direct avec la peau d’autres personnes au niveau des zones d’application pendant environ 60 minutes afin de prévenir la transmission du médicament [12].
Traitements vaginaux à base d'œstrogènes
Les femmes souffrant principalement de sécheresse vaginale peuvent bénéficier d'un traitement ciblé par œstrogènes vaginaux. Ce traitement à faible dose agit sur les symptômes locaux avec des effets minimes ailleurs, le rendant adapté même aux femmes ne pouvant pas suivre un traitement hormonal substitutif systémique [9].
Les formulaires disponibles comprennent :
-
Comprimés/ovules (Vagifem, Vagirux, Gina, Imvaggis) insérés à l'aide d'un applicateur ou avec le doigt
-
Crèmes/gels (Ovestin, Blissel) appliqués avec un applicateur
-
Anneaux (cordon E) insérés pour une libération continue de 90 jours [9] [10]
L’œstrogène vaginal étant très peu absorbé par l’organisme, les femmes ayant un utérus intact peuvent l’utiliser sans progestatif [13]. Des études montrent que la crème d’œstriol réduit la gravité des symptômes de 48 % [12].
Hormones bio-identiques vs hormones synthétiques
Le terme « bio-identique » désigne les hormones dont la structure chimique est identique à celle des hormones produites naturellement par votre corps [11]. Ces options sont disponibles sur ordonnance, que ce soit via le système public ou privé.
L’approche la plus sûre consiste souvent à utiliser des hormones « bio-identiques », c’est-à-dire des hormones dont la structure correspond à celle de vos hormones naturelles, généralement issues de sources végétales comme l’igname mexicaine [4] [12]. Il s’agit notamment de l’œstradiol pour les œstrogènes et de la progestérone micronisée (Utrogestan au Royaume-Uni) [4].
Les préparations plus anciennes contiennent parfois des hormones de synthèse ou des mélanges d'origine animale (comme le Premarin, dérivé de l'urine de juments gestantes) [12]. Certains praticiens estiment que les hormones bio-identiques provoquent moins d'effets secondaires en raison de leur structure similaire [12], bien que la North American Menopause Society mette en garde contre les risques potentiels liés aux préparations magistrales non réglementées [11].
THS à base d'œstrogènes seuls ou combiné
Le choix des hormones adaptées à votre traitement hormonal substitutif (THS) repose sur un facteur essentiel : la présence ou non de votre utérus. Cette décision influence à la fois votre sécurité et l’efficacité du traitement pour la gestion des symptômes de la ménopause .
Quand utilise-t-on un traitement hormonal substitutif (THS) à base d'œstrogènes seuls ?
Vous avez subi une hystérectomie ? Dans ce cas, un traitement hormonal substitutif (THS) à base d’œstrogènes seuls est la solution idéale. Les femmes ayant subi une ablation de l’utérus n’ont pas besoin de progestatifs : leur ajout ne présente aucun avantage [13] [14]. Les œstrogènes seuls suffisent à soulager vos symptômes sans vous exposer à des hormones inutiles.
Cette approche simplifiée est particulièrement efficace pour soulager les bouffées de chaleur , les sueurs nocturnes et la sécheresse vaginale , sans risque de cancer de l'utérus. L'utilisation d'une seule hormone au lieu de deux réduit les risques d'effets secondaires et favorise souvent une meilleure tolérance.
Pourquoi associer œstrogènes et progestatifs ?
Vous avez encore votre utérus ? Un traitement hormonal de substitution combiné est nécessaire pour votre sécurité. Les œstrogènes seuls peuvent entraîner un épaississement anormal de la muqueuse utérine, augmentant légèrement le risque de cancer de l’endomètre [5]. La progestérone agit comme une barrière protectrice, empêchant cette accumulation dangereuse [5].
Votre stade de ménopause détermine l'approche combinée la plus adaptée :
-
La thérapie combinée séquentielle convient aux femmes qui ont eu leurs règles au cours des 12 derniers mois [1].
-
La thérapie combinée continue fonctionne pour les personnes qui n’ont pas eu leurs règles depuis au moins un an [1].
Cette approche combinée vous soulage des symptômes tout en assurant votre sécurité – exactement ce dont vous avez besoin pendant cette transition.
La progestérone micronisée et ses bienfaits
Utrogestan représente la référence en matière de traitement à la progestérone. Contrairement aux anciennes versions synthétiques, ce médicament contient une progestérone identique à celle produite naturellement par l'organisme [15].
Dérivée de plantes comme l’igname ou le soja, la progestérone micronisée offre de réels avantages [16] :
-
Moins d’effets secondaires que les alternatives synthétiques [16]
-
Aucun risque accru de caillot sanguin ou de maladie cardiaque [16]
-
Risque de cancer du sein plus faible pendant les cinq premières années [4]
Cette correspondance « corps identique » signifie que votre corps la reconnaît et la tolère mieux, réduisant ainsi les effets indésirables comme les sautes d’humeur , les ballonnements ou les problèmes de peau [4].
La testostérone dans le cadre d'un traitement hormonal substitutif chez les femmes
Vous pensez que la testostérone est réservée aux hommes ? Détrompez-vous. Les ovaires des femmes produisent en réalité plus de testostérone que d’œstrogènes avant la ménopause [4]. Lorsque ces taux diminuent, certains symptômes persistent malgré un traitement hormonal substitutif classique.
Les recommandations 2024 du NICE préconisent désormais la testostérone pour les femmes présentant une baisse de la libido lorsque le traitement hormonal substitutif classique est insuffisant [17]. Appliquée sous forme de gel ou de crème, elle est absorbée directement par la peau [18].
La testostérone peut aider à bien plus que la simple libido :
-
Énergie et endurance physique accrues [17]
-
Meilleure humeur et moins d’anxiété [17]
-
Pensée plus claire et réduction du brouillard cérébral [17]
-
Des muscles et des os plus forts [17]
-
Amélioration de la qualité du sommeil [17]
Une recherche impliquant 1 200 femmes a révélé que les plus grands avantages de la testostérone se manifestaient dans l’amélioration de l’humeur et de l’anxiété, et pas seulement dans les symptômes sexuels [19].
Les bienfaits du THS qui vont au-delà du soulagement des symptômes
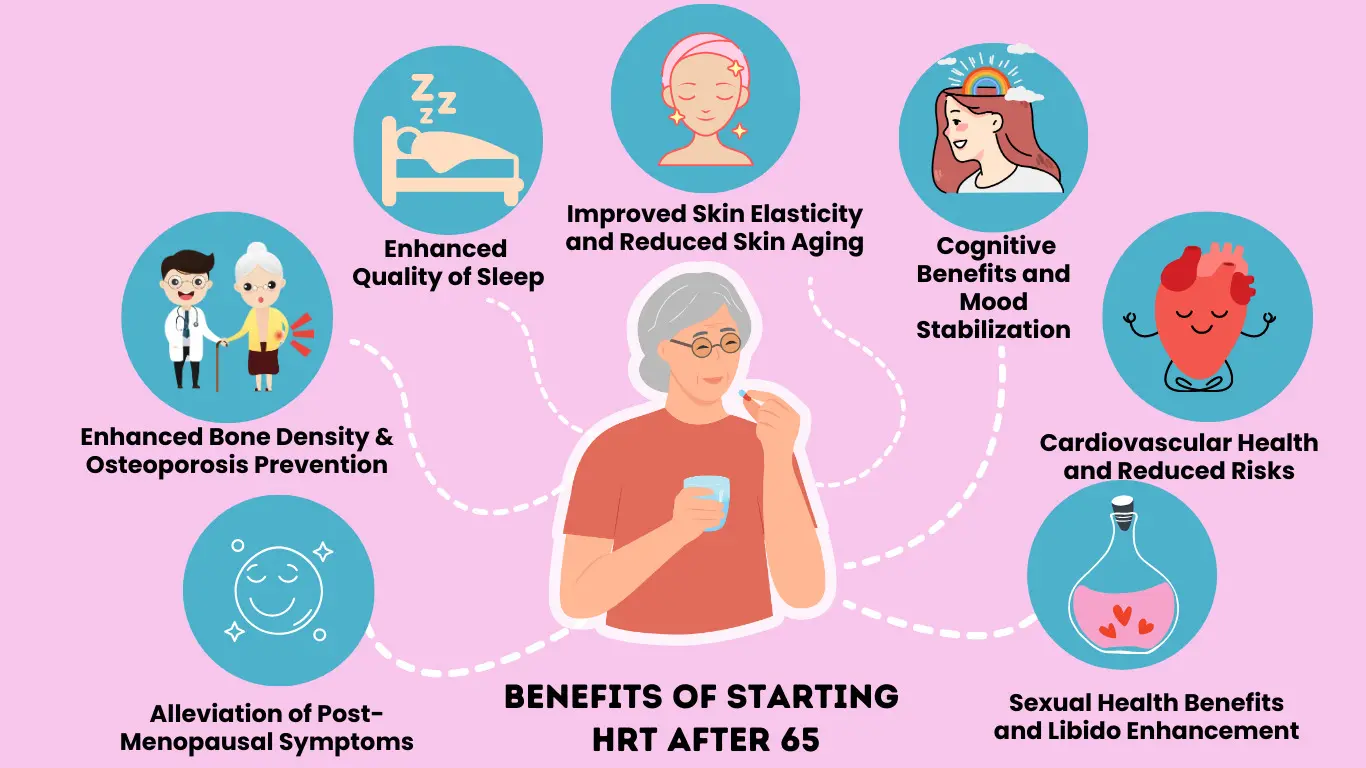
Source de l'image : Amazing Meds
L'hormonothérapie substitutive offre des bienfaits considérables pour la santé, qui vont bien au-delà du simple soulagement des bouffées de chaleur et des sueurs nocturnes. Ces avantages, scientifiquement prouvés, soutiennent de nombreux systèmes de l'organisme et peuvent influencer positivement votre santé à long terme pendant la transition ménopausique .
Des os plus solides et la prévention des fractures
Vos os ont besoin d'œstrogènes pour rester solides et sains. Lorsque le taux d'œstrogènes chute à la ménopause , les femmes peuvent perdre jusqu'à un cinquième de leur densité osseuse en seulement 5 à 7 ans, ce qui augmente considérablement le risque de fracture. Un traitement hormonal substitutif (THS) contribue à maintenir la solidité osseuse et réduit les risques de fractures de la colonne vertébrale et de la hanche [20].
Les femmes ménopausées précocement (avant 45 ans) sont celles qui bénéficient le plus de la protection osseuse offerte par le traitement hormonal substitutif (THS). Les médecins recommandent généralement de poursuivre ce traitement au moins jusqu'à 51 ans afin de prévenir l'ostéoporose et d'autres problèmes de santé [2]. Même les femmes déjà atteintes d'ostéoporose constatent des effets bénéfiques sur le renforcement osseux, réduisant significativement leur risque de fracture [2].
Les recherches soutenant l’HRT pour la santé osseuse sont impressionnantes : des études montrent qu’elle peut augmenter la densité osseuse d’environ 7 % sur deux ans et réduire les fractures de la colonne vertébrale d’un tiers [21].
Protection de la santé cardiaque et réduction du risque de maladie
Vous souhaitez protéger votre cœur pendant la ménopause ? Le traitement hormonal substitutif (THS) apporte des bénéfices cardiovasculaires importants lorsqu’il est instauré au bon moment. Le facteur clé est le timing : les œstrogènes sont bénéfiques pour la santé des vaisseaux sanguins, mais peuvent ne pas être efficaces en cas de maladie cardiaque déjà installée [8].
Les femmes qui commencent un traitement hormonal substitutif dans les 10 ans suivant la ménopause et avant l'âge de 60 ans constatent des améliorations remarquables de leur santé cardiaque :
-
Réduction de 32 % des maladies coronariennes [8]
-
Jusqu’à 52 % de réduction du risque de maladie cardiovasculaire après 10 ans de traitement [8]
-
mortalité toutes causes confondues en baisse de 39 % [8]
L’hormonothérapie substitutive (HTS) réduit également de 20 à 30 % le nombre de nouveaux cas de diabète, offrant ainsi une protection métabolique supplémentaire [8]. La British Heart Foundation note que l’HTS peut améliorer le taux de cholestérol, bien que certaines formulations puissent avoir des effets variables [22].
Meilleure humeur, meilleur sommeil et meilleure clarté mentale
Vous souffrez de brouillard mental ou de changements d'humeur ? Le THS peut améliorer les fonctions cognitives, même si la recherche continue d'explorer son plein potentiel dans la prévention de la démence.
L’œstradiol contribue à réguler des neurotransmetteurs clés liés à la dépression : la sérotonine, la dopamine et la noradrénaline [6]. Ceci explique pourquoi le traitement hormonal substitutif (THS) améliore souvent les sautes d’humeur pendant la ménopause. Une étude a montré que les femmes prenant des œstrogènes et de la progestérone étaient significativement moins susceptibles de souffrir de dépression que celles sous placebo (17,3 % contre 32,3 %) [6].
La qualité du sommeil s'améliore également, car le THS réduit les sueurs nocturnes qui perturbent fréquemment le repos. Un meilleur sommeil favorise naturellement les fonctions cognitives et le bien-être émotionnel.
Force musculaire accrue et peau d'apparence plus jeune
Le traitement hormonal substitutif (THS) contribue à préserver la force musculaire pendant la transition ménopausique. Le NHS confirme que l'hormonothérapie peut améliorer la force musculaire et aider à maintenir une bonne masse musculaire lorsqu'elle est associée à une activité physique régulière [3].
Votre peau bénéficie grandement d'un traitement aux œstrogènes :
-
Hydratation accrue et sécheresse réduite [23]
-
Teneur en collagène améliorée — jusqu’à 48 % d’augmentation dans certaines études [23]
-
Épaisseur et élasticité améliorées [23]
-
Moins de rides et une meilleure apparence générale [24]
Des recherches montrent que les femmes ménopausées sous traitement hormonal substitutif (THS) ont une peau significativement plus épaisse que celles qui ne suivent aucun traitement [23]. Des études révèlent également une meilleure rétention d'eau et une fonction barrière améliorée au niveau de la couche externe de la peau [23].
Ces nombreux avantages montrent pourquoi les professionnels de la santé considèrent le THS comme bien plus qu'une simple gestion des symptômes : c'est une protection pour de multiples systèmes de l'organisme pendant la transition ménopausique.
Risques et effets secondaires du THS

Source de l'image : The Pharmaceutical Journal
Comme tout médicament, le traitement hormonal de la ménopause (THM) comporte certains risques, en plus de ses avantages. Comprendre ces risques potentiels vous permettra de prendre des décisions éclairées concernant le traitement de la ménopause le mieux adapté à votre situation.
Cancer du sein : que disent les données probantes ?
Les recherches montrent une légère augmentation du risque de cancer du sein associée à l'utilisation d'un traitement hormonal substitutif (THS). Les femmes suivant un THS combiné pendant 5 ans présentent environ 5 cas supplémentaires pour 1 000 femmes [3]. Le risque dépend du type de THS choisi : le traitement combiné (œstrogènes et progestatifs) comporte des risques plus élevés que le THS à base d'œstrogènes seuls [25]. Chez les femmes ayant subi une hystérectomie sous traitement à base d'œstrogènes seuls, les études montrent une augmentation faible, voire nulle, du risque de cancer du sein [3].
Risque de caillots sanguins et d'AVC
Le mode d'administration a une incidence majeure. Les comprimés d'hormonothérapie substitutive (HTS) augmentent légèrement le risque de formation de caillots sanguins et d'AVC [3]. Les patchs, gels et sprays fonctionnent différemment : ils diffusent les hormones à travers la peau, contournant ainsi le foie et ne présentant pas de risque accru de formation de caillots [26]. C'est pourquoi les femmes présentant un risque élevé de formation de caillots se voient généralement recommander des options transdermiques plutôt que des comprimés [3].
Problèmes de vésicule biliaire et de foie
Les utilisatrices d'un traitement hormonal substitutif (THS) présentent un risque accru de maladies de la vésicule biliaire, des études montrant une incidence plus élevée de calculs biliaires quel que soit le type d'hormone [27]. Cependant, le traitement transdermique présente un risque beaucoup plus faible de maladies de la vésicule biliaire que les formes orales (1,3 contre 2,0 pour 100 femmes sur cinq ans) [28]. Pour 140 femmes choisissant les patchs plutôt que les comprimés sur une période de cinq ans, une cholécystectomie pourrait potentiellement être évitée [29].
Démence et risques cognitifs
Les recherches sur la démence restent mitigées. Certaines études suggèrent que les œstrogènes pourraient réduire le risque de démence, tandis que d'autres indiquent une augmentation potentielle [30]. Une vaste étude danoise a révélé que l'hormonothérapie pourrait accroître le risque de démence plus tard dans la vie [31]. Le moment du traitement semble crucial : commencer un THS après 65 ans paraît plus susceptible d'influencer le risque cognitif qu'un traitement plus précoce [32].
Effets secondaires courants et comment les gérer
La plupart des effets secondaires disparaissent dans les trois mois suivant le début d'un THS [7]. Les effets indésirables courants liés aux œstrogènes incluent les maux de tête, la sensibilité mammaire et les saignements vaginaux inattendus [7]. Les progestatifs peuvent provoquer des changements d'humeur, des nausées et une éruption cutanée légère [7]. La bonne nouvelle ? La plupart des femmes ne présentent aucun effet secondaire ou seulement des effets mineurs [7]. Malgré les inquiétudes concernant la prise de poids, les données suggèrent une association minime avec la plupart des types de THS [7].
Si la sensibilité mammaire ou les saignements inattendus persistent au-delà de six mois, consultez votre professionnel de santé afin d'ajuster votre dosage ou de changer de type de THS [33]. En cas de nausées, la prise des comprimés au cours des repas et le fait de privilégier des repas simples le temps que votre corps s'adapte sont généralement efficaces [33].
Qui devrait et ne devrait pas prendre un traitement hormonal de substitution (THS).
L’hormonothérapie n’est pas sans risque pour toutes les femmes. Certaines pathologies la rendent inadaptée et nécessitent une évaluation approfondie avant tout traitement.
Affections médicales pouvant empêcher l'utilisation d'un THS
Certaines femmes présentent des risques plus élevés liés à l'hormonothérapie substitutive . Il s'agit notamment des femmes atteintes de :
-
Antécédents de cancers hormono-dépendants comme le cancer du sein, de l'endomètre ou de l'ovaire
-
Thromboembolie veineuse active ou récente (caillots sanguins)
-
Hypertension artérielle non traitée
-
maladie hépatique active
-
Saignements vaginaux non diagnostiqués
Les femmes souffrant de ménopause précoce bénéficient généralement d'un THS jusqu'à au moins l'âge naturel de la ménopause (51 ans), sauf en cas de contre-indications.
Quand envisager des alternatives
Vous ne pouvez pas prendre un traitement hormonal de substitution en toute sécurité ? Plusieurs options efficaces peuvent vous aider à gérer vos symptômes :
-
Antidépresseurs pour les bouffées de chaleur et les sueurs nocturnes
-
Hydratants vaginaux pour la sécheresse vaginale
-
Des changements de mode de vie pour favoriser la santé osseuse et gérer la prise de poids
-
Les remèdes naturels comme la thérapie cognitivo-comportementale pour les sautes d'humeur
Discutez de votre admissibilité avec votre médecin
Votre médecin généraliste a besoin d'informations complètes pour vous recommander le traitement le plus sûr. Préparez-vous à en discuter :
-
Antécédents médicaux complets
-
Antécédents familiaux de cancer ou de troubles de la coagulation
-
Symptômes actuels affectant votre qualité de vie après la ménopause
-
Préférences personnelles concernant les alternatives au THS
Des bilans réguliers restent essentiels tout au long du traitement afin de réévaluer les bénéfices par rapport aux risques à mesure que vos besoins de santé évoluent.
Conclusion
Les données scientifiques sont formelles : le THS peut transformer la vie des femmes confrontées aux symptômes de la ménopause . De la réduction des bouffées de chaleur et des sueurs nocturnes à la protection de la santé osseuse et au soutien de la santé cardiovasculaire , le traitement hormonal substitutif offre des solutions concrètes au moment où vous en avez le plus besoin.
Vos options n'ont jamais été aussi nombreuses. Les patchs, gels et sprays éliminent les risques de formation de caillots sanguins associés aux comprimés, tandis que les hormones bio-identiques, comme la progestérone micronisée, présentent moins d'effets secondaires que les anciennes versions synthétiques. Les études montrent systématiquement que les bénéfices du THS l'emportent sur les risques pour la plupart des femmes, surtout lorsqu'il est débuté avant 60 ans ou dans les 10 ans suivant la ménopause .
Certaines femmes ne peuvent pas suivre un traitement hormonal substitutif (THS) en raison de cancers hormono-dépendants ou de troubles de la coagulation. Si c'est votre cas, rassurez-vous : il existe des alternatives au THS pour soulager les symptômes, même si leur efficacité est généralement moins constante. Les femmes ménopausées précocement bénéficient généralement d'un THS jusqu'à au moins 51 ans, sauf contre-indication médicale.
La clé du succès réside dans un traitement personnalisé. Des consultations régulières avec votre professionnel de santé garantissent que votre traitement reste adapté à l'évolution de vos besoins. Tenez compte de la gravité de vos symptômes, de vos antécédents médicaux et de vos préférences personnelles pour prendre vos décisions. Si les remèdes naturels contre la ménopause peuvent soulager certaines femmes, ils sont souvent moins efficaces qu'un traitement hormonal.
La plupart des femmes constatent une nette amélioration de leur qualité de vie une fois qu'elles ont trouvé le traitement hormonal de substitution qui leur convient, disant adieu aux sautes d'humeur et aux troubles de la concentration . Ne laissez pas les symptômes de la ménopause vous empêcher de profiter pleinement de la vie après la ménopause .
Prête à explorer vos options ? Prenez rendez-vous avec votre médecin généraliste ou un spécialiste de la ménopause. Ils pourront évaluer votre situation et élaborer un plan de traitement adapté à votre corps et à votre mode de vie. Vous méritez de vous sentir au mieux de votre forme durant cette importante transition.
Points clés à retenir
Comprendre les options de THS et leurs avantages peut aider les femmes à prendre des décisions éclairées concernant la gestion des symptômes de la ménopause et la protection de leur santé à long terme.
• Le THS traite efficacement 80 % des symptômes de la ménopause : bouffées de chaleur, sueurs nocturnes et sécheresse vaginale s’améliorent souvent quelques semaines après le début du traitement.
• Les options transdermiques (patchs, gels, sprays) sont plus sûres que les comprimés : elles n’augmentent pas le risque de formation de caillots sanguins et sont recommandées pour les femmes présentant un risque plus élevé de MTEV.
• Les hormones identiques à celles du corps, comme la progestérone micronisée, provoquent moins d'effets secondaires : elles correspondent aux structures hormonales naturelles et réduisent les risques par rapport aux alternatives synthétiques.
• Commencer un THS avant l'âge de 60 ans offre une protection cardiovasculaire - Une initiation précoce réduit le risque de maladie cardiaque de 32 % et la mortalité globale de 39 %.
• Le risque de cancer du sein est faible mais réel – le THS combiné ajoute environ 5 cas pour 1 000 femmes sur 5 ans, mais les avantages l’emportent souvent sur les risques.
La clé du succès d'un traitement hormonal de substitution réside dans des plans de traitement personnalisés qui tiennent compte des antécédents médicaux, de la gravité des symptômes et des préférences de chaque patiente. Des consultations médicales régulières garantissent un dosage optimal et une sécurité maximale tout au long du traitement.
FAQ
Q1. Quels sont les principaux types de THS disponibles au Royaume-Uni ? Les principaux types de THS au Royaume-Uni comprennent les comprimés, les patchs, les gels, les sprays et les traitements vaginaux. Les comprimés et les patchs sont des options courantes, tandis que les gels et les sprays sont de plus en plus utilisés. Les traitements vaginaux sont indiqués pour les symptômes localisés.
Q2. Combien de temps faut-il généralement pour que le THS fasse effet ? La plupart des femmes constatent une amélioration de leurs symptômes de ménopause quelques semaines après le début du THS. Cependant, il faut parfois jusqu’à trois mois pour en ressentir tous les bienfaits et pour que les effets secondaires disparaissent.
Q3. L’hormonothérapie substitutive peut-elle améliorer la santé osseuse pendant la ménopause ? Oui, l’hormonothérapie substitutive peut améliorer significativement la santé osseuse pendant la ménopause. Elle contribue au maintien de la densité osseuse et réduit le risque d’ostéoporose et de fractures, ce qui est particulièrement bénéfique pour les femmes ménopausées précocement ou prématurément.
Q4. Le THS présente-t-il des avantages cardiovasculaires ? Le THS peut offrir des avantages cardiovasculaires s’il est instauré dans les 10 ans suivant la ménopause ou avant l’âge de 60 ans. Il peut réduire le risque de maladie coronarienne et diminuer la mortalité cardiovasculaire globale chez ces femmes.
Q5. Quels sont les principaux risques associés à un traitement hormonal substitutif (THS) ? Les principaux risques associés à un THS comprennent une légère augmentation du risque de cancer du sein avec un THS combiné et une légère augmentation du risque de thrombose avec un THS oral. Toutefois, ce risque varie selon le type de THS, son mode d’administration et l’état de santé de chaque personne.
Références
[1] - https://www.newsonhealth.co.uk/knowledge/hormone-replacement-therapy-the-benefits-and-risks-of-hrt
[2] - https://www.bbc.co.uk/news/health-62336456
[3] - https://www.menopausecare.co.uk/blog/hrt-risks-and-benefits
[4] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/types-of-hormone-replacement-therapy-hrt/
[5] - https://www.forthwithlife.co.uk/blog/menopause-hormones/
[6] - https://www.ncbi.nlm.nih.gov/books/NBK493191/
[7] - https://www.nhs.uk/conditions/menopause/treatment/
[8] - https://my.clevelandclinic.org/health/treatments/15245-hormone-therapy-for-menopause-symptoms
[9] - https://www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372
[10] - https://nhssomerset.nhs.uk/prescribing-and-medicines-management/prescribing-guidelines-by-clinical-area/menopause-and-hormone-replacement-therapy/oral-hormone-replacement-therapy/
[11] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/
[12] - https://nhssomerset.nhs.uk/prescribing-and-medicines-management/prescribing-guidelines-by-clinical-area/menopause-and-hormone-replacement-therapy/transdermal-hormone-replacement-therapy/
[13] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/oestrogen-tablets-patches-gel-and-spray/about-oestrogen-tablets-patches-gel-and-spray/
[14] - https://onlinedoctor.superdrug.com/hrt-patches.html
[15] - https://healthinmenopause.co.uk/hrt-the-different-types/
[16] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/vaginal-oestrogen/about-vaginal-oestrogen/
[17] - https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/diagnosis-treatment/drc-20352294
[18] - https://onlinedoctor.superdrug.com/hormone-replacement-therapy.html
[19] - https://www.health.harvard.edu/womens-health/are-bioidentical-hormones-superior-to-hormone-medications
[20] - https://themenopausecharity.org/information-and-support/what-can-help/treatment-options/types-of-hrt/
[21] - https://hormoneclinic.uk/bhrt-vs-hrt-whats-the-difference/
[22] - https://menopause.org.au/hp/information-sheets/oestrogen-only-mht
[23] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/continuous-combined-hormone-replacement-therapy-hrt-tablets-capsules-and-patches/about-continuous-combined-hrt/
[24] - https://theros.org.uk/information-and-support/osteoporosis/treatment/hormone-replacement-therapy/
[25] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/utrogestan-micronised-progesterone/about-utrogestan/
[26] - https://www.drlouisenewson.co.uk/knowledge/utrogestan-micronised-progesterone-explained
[27] - https://www.newsonhealth.co.uk/testostérone-pour-les-femmes
[28] - https://www.drlouisenewson.co.uk/knowledge/the-importance-of-testosterone-for-women
[29] - https://thebms.org.uk/publications/consensus-statements/prevention-and-treatment-of-osteoporosis-in-women/
[30] - https://www.nhs.uk/conditions/osteoporosis/treatment/
[31] - https://www.drlouisenewson.co.uk/knowledge/can-hrt-and-testosterone-prevent-osteoporosis
[32] - https://pmc.ncbi.nlm.nih.gov/articles/PMC9178928/
[33] - https://www.bhf.org.uk/informationsupport/support/women-with-a-heart-condition/menopause-and-heart-disease
[34] - https://pmc.ncbi.nlm.nih.gov/articles/PMC6843314/
[35] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/benefits-and-risks-of-hormone-replacement-therapy-hrt/
[36] - https://gremjournal.com/journal/01-2024/menopause-and-the-effects-of-hormone-replacement-therapy-on-skin-ageing-a-short-review/
[37] - https://www.healthline.com/health/skin/hrt-skin-effects
[38] - https://bmjgroup.com/study-provides-new-estimates-of-breast-cancer-risks-associated-with-hrt/
[39] - https://www.drlouisenewson.co.uk/knowledge/blood-clot-and-hrt-what-you-need-to-know
[40] - https://pmc.ncbi.nlm.nih.gov/articles/PMC10695378/
[41] - https://www.sciencedaily.com/releases/2008/07/080710193709.htm
[42] - https://www.bmj.com/content/337/bmj.a386
[43] - https://www.alzheimers.org.uk/about-dementia/managing-the-risk-of-dementia/additional-treatments-for-dementia-risk/hormones
[44] - https://www.alzheimersresearchuk.org/news/link-between-hormone-replacement-therapy-and-increased-risk-of-dementia-in-later-life/
[45] - https://www.cnn.com/2023/11/02/health/hormone-replacement-dementia-wellness
[46] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/side-effects-of-hormone-replacement-therapy-hrt/
[47] - https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/continuous-combined-hormone-replacement-therapy-hrt-tablets-capsules-and-patches/side-effects-of-continuous-combined-hrt/




